When people hear the term HPV, they immediately think of adults, Pap smears, and cervical cancer screenings. But one of the most overlooked facts in pediatric medicine is this:
HPV infections can and do occur in children and adolescents — often silently.
This doesn’t mean something catastrophic has happened.
It means parents need accurate information, not fear.
This comprehensive guide explains how HPV spreads to young people, what symptoms to watch for, the real risks, treatment options, the role of the immune system, when to consider possible abuse, and why the HPV vaccine is one of the strongest protections you can give your child.
What Is HPV? A Straightforward Explanation
HPV (Human Papillomavirus) is a huge family of viruses — over 200 different types — divided into three main groups:
1. Cutaneous HPV (skin types)
-
Hand warts
-
Plantar warts
-
Flat warts
These are extremely common in children.
2. Low-risk mucosal HPV
-
Genital warts
-
Oral warts
-
Throat papillomas
These are uncomfortable, but not linked to cancer.
3. High-risk HPV
These strains can cause:
-
Cervical cell changes
-
Anal cell changes
-
Penile cell changes
-
Vaginal cell changes
-
Oropharyngeal (throat/tonsil) cell changes
High-risk strains only become dangerous when infections persist for years.
How Children Actually Get HPV
Most people incorrectly believe HPV can only be transmitted sexually.
This is not true, especially for children.
Below are the real, documented routes:
1. Skin-to-Skin Contact (Most Common in Children)
Kids are constantly:
-
Touching shared surfaces
-
Playing contact games
-
Touching their faces and mouths
-
Sharing toys
HPV spreads extremely easily through this type of ordinary contact — especially strains that cause skin warts.
2. Household Transmission
HPV DNA has been found on:
-
Towels
-
Razors
-
Bathroom surfaces
-
Toothbrushes
-
Toys
-
Phones
-
Shared cosmetics
Many homes have at least one person carrying some form of HPV.
Children pick it up naturally.
3. Vertical Transmission During Childbirth
Infants can acquire HPV from their mother’s birth canal.
This may later cause:
-
Oral warts
-
Throat HPV
-
Skin warts
-
Rarely, recurrent respiratory papillomatosis (RRP)
4. Auto-Inoculation (Self-Transfer)
If a child has a wart on the hand, they may touch:
-
Their mouth
-
Their genitals
-
Their face
-
Any other skin area
This spreads HPV from one body site to another.
5. Normal Teen Exposure
Most HPV exposures in life occur during adolescence, because:
-
Social contact increases
-
Hormonal changes affect immunity
-
Teens explore relationships
-
Skin-to-skin contact becomes more common
More than 80% of all people will acquire HPV in their lifetime.
Symptoms of HPV in Children and Adolescents
Most HPV infections are completely silent.
But when symptoms appear, they may include:
In Children
-
Hand warts
-
Plantar warts
-
Flat warts (face)
-
Oral warts
-
Genital warts (rare but possible through non-sexual routes)
In Adolescents
-
Genital warts
-
Oral bumps or irritation
-
Throat symptoms
-
Abnormal Pap smear (if early screening is done)
High-risk HPV
Has no visible symptoms.
It silently affects cell structure over months or years.
Important and Rare: Considering the Possibility of Sexual Abuse
This subject cannot be ignored.
Although many HPV cases in children occur through normal, non-sexual transmission, medical guidelines require doctors to evaluate all possibilities, including sexual abuse, when:
-
A young child develops genital HPV
-
There are recurrent genital warts
-
The pattern of infection does not match their age
This does not automatically mean abuse occurred.
But trained specialists must evaluate the situation to ensure a child’s safety.
These evaluations are done respectfully, privately, and professionally.
Is HPV Dangerous in Children?
For most children, no.
-
Cutaneous HPV = harmless but annoying
-
Low-risk HPV = treatable
-
High-risk HPV = rare in children
In Teenagers
High-risk HPV becomes more relevant, but even then:
90% of adolescent infections clear naturally within 1–2 years.
Only persistent, long-term, high-risk infections can cause problems later in life.
How the Immune System Clears HPV
The immune system plays the biggest role in defeating HPV.
Clearance timelines:
-
Children: 6–18 months
-
Teens: 6–24 months
-
Adults: 6–48 months
Younger bodies are often better at clearing HPV quickly.
This is why immune health matters.
Diagnosis: How HPV Is Identified in Young People
Children
-
Visual diagnosis by pediatrician or dermatologist
-
ENT specialists for oral/throat lesions
-
Pediatric gynecology/urology for genital warts
Adolescents
-
Visual exam
-
HPV DNA testing
-
Pap smear (not routine until 21, but possible earlier if needed)
-
Colposcopy for abnormal results
Treatment Options for Children & Teens
1. Watchful Waiting
Most warts and mild infections clear without intervention.
2. Wart Removal
-
Cryotherapy
-
Laser removal
-
Topical acids
-
Prescription creams
-
Surgical removal (rare)
3. Lifestyle & Immune Support
Parents often focus on:
-
Sleep
-
Diet
-
Vitamin D
-
Stress reduction
-
Probiotics
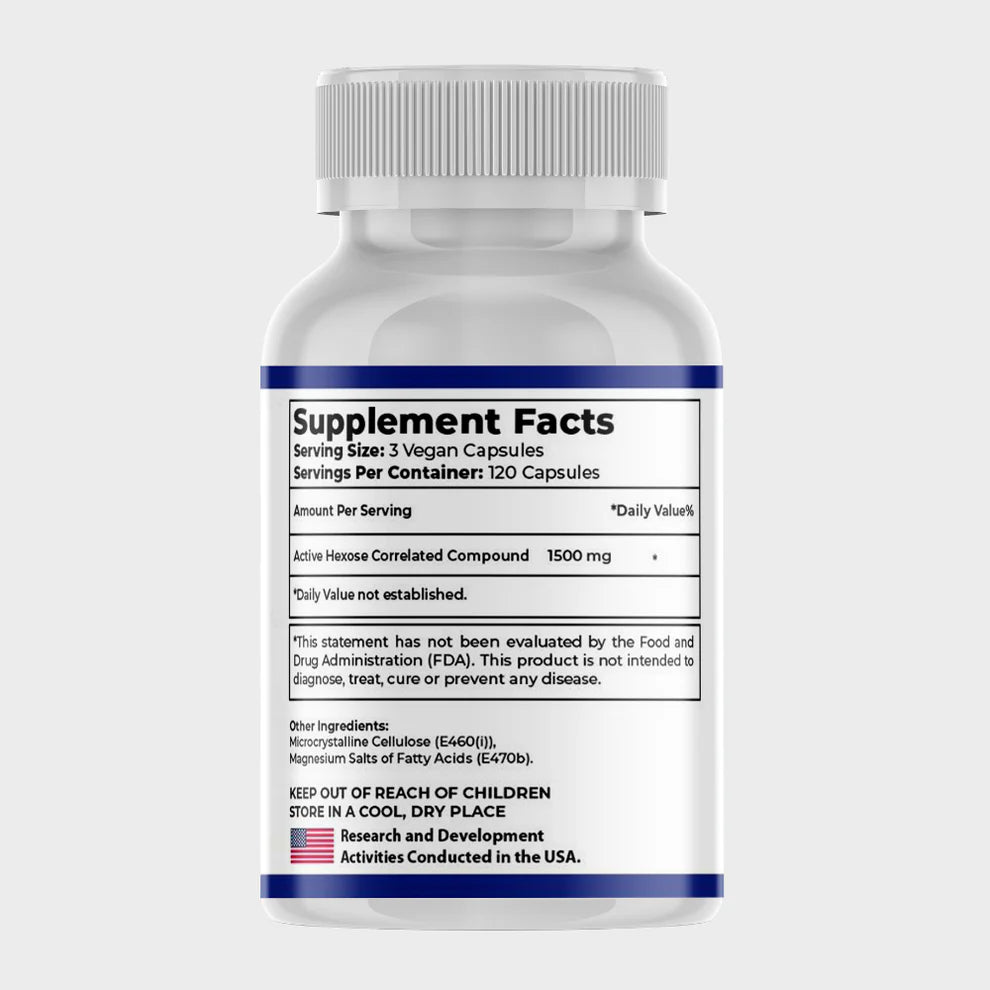
Supplements like AHCC have research supporting HPV immune clearance in both adults and adolescents.
4. Treating Oral or Genital HPV
Handled by specialists:
-
Dermatologists
-
Pediatric gynecologists
-
Pediatric urologists
-
ENT doctors
Treatment success rates are high when combined with immune support.
HPV in Adolescence: Why Awareness Matters Most Here
Teenagers have the highest HPV exposure rates.
Common factors include:
-
Puberty
-
Dating behaviors
-
Hormonal changes
-
Social environments
-
Shared items
Even high-risk HPV infections typically clear naturally — but they must be monitored.
Cancer Risk: The Real Science
Cancer develops only when:
-
The HPV strain is high-risk
-
The infection persists for years
-
Abnormal cells go untreated
Children: extremely low risk
Teens: low but not zero
Adults: higher risk due to persistence
This is where the HPV vaccine becomes critical.
The HPV Vaccine: The Most Powerful Protection You Can Give Your Child
This deserves its own section.
The HPV vaccine protects against:
-
Cervical cancer
-
Vaginal cancer
-
Anal cancer
-
Penile cancer
-
Throat (oropharyngeal) cancer
-
Genital warts
-
Most high-risk HPV strains
Recommended Schedule
-
Ages 9–14 → 2 doses
-
Ages 15–26 → 3 doses
Vaccinating before exposure gives the strongest immune protection.
One of the most important facts:
The HPV vaccine does not treat an existing infection,
but it prevents other strains — and there are many.
This dramatically reduces lifetime cancer risk.
The vaccine is safe, well-studied, and globally recommended.
Every major medical organization supports it:
-
WHO
-
CDC
-
American Cancer Society
-
AAP (American Academy of Pediatrics)
If there is one preventive step parents should not skip, it is this vaccine.
When Should a Parent Seek Medical Help?
Seek evaluation if your child has:
-
Genital bumps
-
Oral or throat lesions
-
Rapidly growing warts
-
Recurrent warts
-
Unusual symptoms
-
Abnormal cervical screening
-
Any concerns about exposure
Early evaluation gives clarity and peace of mind.
Long-Term Outlook: Very Good When Managed Properly
For most children and adolescents:
-
HPV is temporary
-
The immune system clears it
-
Complications are rare
-
Treatments are effective
-
Monitoring protects long-term health
-
The HPV vaccine prevents future problems
Knowledge plus prevention equals safety.
Final Thoughts
HPV infection in young people is far more common — and far less dangerous — than most parents realize when handled correctly.
Understanding:
-
how HPV spreads,
-
how to identify symptoms,
-
when to seek help,
-
how to support the immune system,
-
and the protective power of the vaccine
gives parents everything they need to protect their child now and as they grow older.
Informed parents are empowered parents.