This article provides an in-depth exploration of the Human Papillomavirus (HPV) vaccine, addressing critical aspects such as its mechanism, effectiveness, recommended recipients, side effects, and more. Click on a topic below to jump to that section.
- What Is the HPV Vaccine?
- How Does the HPV Vaccine Work?
- Who Should Get the HPV Vaccine?
- What Are the Side Effects of the HPV Vaccine?
- How Many Doses of HPV Vaccine Are Needed?
- Is the HPV Vaccine Safe?
- Can Males Also Receive the HPV Vaccine?
- How Effective Is the HPV Vaccine?
- At What Age Should the HPV Vaccine Be Given?
- Can the HPV Vaccine Cause HPV?
- Can the HPV Vaccine Prevent Cervical Cancer?
- Is the HPV Vaccine Necessary If I Am Already Sexually Active?
- Does the HPV Vaccine Protect Against All Types of HPV?
- Is the HPV Vaccine Free of Cost?
- Can I Get the HPV Vaccine If I Already Have HPV?
- How Long Does the HPV Vaccine Last?
- What Are the Ingredients in the HPV Vaccine?
- Can the HPV Vaccine Help If I Already Have Genital Warts?
- Is the HPV Vaccine Only for Females?
- Can Pregnant Women Receive the HPV Vaccine?
What Is the HPV Vaccine?
The HPV vaccine is a major advancement in preventive medicine, targeting the Human Papillomavirus (HPV), a common sexually transmitted infection linked to various cancers like cervical, anal, and oropharyngeal cancers.
Several HPV vaccines exist, including Gardasil, Gardasil 9, and Cervarix. Gardasil covers four HPV types, while Gardasil 9 protects against nine types. Cervarix targets the two most linked to cervical cancer.
Administered in a series, the CDC recommends vaccination at 11-12, but as early as 9. Catch-up shots are suggested up to age 21 for males and 26 for females, with high-risk groups up to 45.
The vaccine effectively reduces cervical precancers and HPV-related diseases, including genital warts and cervical cancer.
Extensively researched, the HPV vaccine is safe, with mostly mild side effects. Its safety remains monitored globally.
The vaccine boosts the immune system to produce antibodies against HPV, preventing infection but not treating existing ones.
Challenges to vaccine uptake include lack of awareness and misconceptions. Efforts aim to boost vaccination rates.
The HPV vaccine is integrated into many countries' vaccination programs, lessening the HPV-related disease burden.
Ongoing research explores next-gen vaccines, broader coverage, long-term effectiveness, and expanding usage to other age groups.
How Does the HPV Vaccine Work?
The HPV vaccine is a crucial tool against the widespread Human Papillomavirus (HPV) infection, primarily a sexually transmitted ailment. HPV comprises over 100 strains, with some leading to genital warts and cancers. The vaccine's primary role is to provide immunity against these high-risk strains.
HPV vaccines are preventive, not curative, working by training the immune system to fight the virus if exposed in the future. They employ virus-like particles (VLPs) that mimic HPV's outer shell but lack its DNA. VLPs are harmless and can't cause infection, but they stimulate antibody production.
When administered, the vaccine prompts the immune system to treat VLPs as invaders. Antibodies are created to combat HPV, forming a long-lasting immune response.
If a vaccinated person encounters the actual HPV later, their primed immune system swiftly recognizes and neutralizes it, preventing infection and related health issues.
Extensive research shows the vaccine's efficacy in reducing infections and diseases caused by targeted HPV strains.
The vaccine is given through a series of injections, with the schedule based on age and health status. It offers long-term protection, reducing HPV-related disease risks into adulthood.
While most effective before sexual activity starts, it still benefits those exposed to HPV. Widespread vaccination fosters herd immunity, protecting even the unvaccinated, contributing to HPV control efforts.
Who Should Get the HPV Vaccine?
The Human Papillomavirus (HPV) vaccine is a significant step forward in public health, targeting a virus linked to several cancers and other health conditions. Understanding who should receive this vaccine is crucial for maximizing its protective benefits. The vaccine is primarily recommended for preteens and teenagers, but the guidelines extend to other age groups as well.
Preteen vaccination is a cornerstone of HPV prevention strategy. The Centers for Disease Control and Prevention (CDC) recommends the vaccine for girls and boys at the age of 11 or 12. This timing is critical as it ensures the vaccine is administered before potential exposure to HPV through sexual contact, and because the immune response to the vaccine is stronger at this younger age.
Teenagers and young adults who missed the initial vaccination window are also advised to receive the vaccine. Females can get vaccinated through age 26, and males through age 21. The vaccine remains beneficial in this age group, offering protection against strains of HPV they may not have been exposed to.
Men who have sex with men and transgender individuals are recommended to get vaccinated through age 26. This recommendation is due to the higher risk of HPV exposure and related health complications in these populations. The vaccine provides a critical defense against HPV-related diseases, including certain types of cancer.
Individuals with compromised immune systems, including those with HIV, are also advised to get vaccinated through age 26. A weakened immune system can increase vulnerability to HPV and its complications, making vaccination an important protective measure.
Some adults aged 27 through 45 years who have not been previously vaccinated may also benefit from receiving the HPV vaccine. This recommendation is based on a discussion with their healthcare provider, as the likelihood of new HPV exposure decreases with age and sexual activity.
It's important to note that the HPV vaccine is not just for females. Males are equally at risk for HPV infections and related diseases, such as genital warts and certain cancers. Vaccinating boys contributes to herd immunity, reducing the overall prevalence of HPV in the population.
Pregnant women are typically advised to delay HPV vaccination until after pregnancy. While there is no evidence that the vaccine poses harm during pregnancy, postponement is a precautionary measure. Women who find out they are pregnant after starting the vaccine series are advised to complete it after pregnancy.
For individuals with a history of HPV-related diseases, such as genital warts or cervical precancer, the vaccine can still offer benefits. While it doesn't treat existing infections, it can provide protection against other HPV strains not previously encountered.
Finally, people with a severe allergy to any component of the HPV vaccine should not receive it. It's important for individuals to discuss their medical history with a healthcare provider to ensure the HPV vaccine is safe for them.
What Are the Side Effects of the HPV Vaccine?
The HPV vaccine, crucial for cancer and genital warts prevention, is generally safe but can cause side effects. Understanding them is vital:
-
Common side effects: Pain, redness, or swelling at the injection site, mild fever, headaches, and fatigue. These are short-lived and typically resolve without specific treatment.
-
Nausea, dizziness, or fainting: Occurs, especially in teenagers. Staying seated or lying down for 15 minutes post-vaccination reduces fainting risk.
-
Muscle or joint pain: Occasionally reported, typically mild, and temporary. Over-the-counter pain relievers can help.
-
Allergic reaction: Rare but requires immediate medical attention. Symptoms include hives, swelling, difficulty breathing, rapid heartbeat, dizziness, and weakness.
-
Guillain-Barre Syndrome (GBS): Very rare and not directly linked to the HPV vaccine, as per studies.
-
Autoimmune diseases: No consistent evidence links the HPV vaccine to autoimmune diseases, as extensive research has shown.
-
Menstrual cycle changes: Some females reported changes, with ongoing research but no conclusive evidence of a direct link.

How Many Doses of HPV Vaccine Are Needed?
The HPV vaccine is crucial for preventing specific cancers and genital warts from HPV. The dosing schedule depends on age and factors like immune health:
-
Under 15 years old: A two-dose schedule with the first shot and a second dose 6-12 months later is recommended.
-
15 years or older, or with weakened immune systems: A three-dose series, with the initial shot, a second dose 1-2 months later, and a third dose 6 months after the first.
-
Starting at age 11-12, or as early as 9: Follow guidelines from health authorities for the first dose.
-
Adherence to recommended intervals is crucial. Interruptions don't require restarting, but doses should be given promptly.
-
For those receiving the first dose before 15 but with over 12 months between doses, a third dose is often recommended.
-
Special populations, like those with immunocompromising conditions, may need a three-dose schedule.
-
Pregnant women should delay remaining doses until after pregnancy, with no evidence of harm to the fetus.
-
Ensure all doses are of the same vaccine brand for consistency.

Is the HPV Vaccine Safe?
The Human Papillomavirus (HPV) vaccine, a pivotal tool in preventing specific cancers and genital warts, is subject to rigorous safety testing and continuous monitoring. It stands as one of the most extensively studied vaccines to date.
One of the primary concerns surrounding any vaccine revolves around the risk of severe allergic reactions. Fortunately, the HPV vaccine records exceedingly rare instances of such reactions. The estimated occurrence of anaphylaxis, a severe allergic response, is roughly 1.7 cases per million doses, a rate consistent with other vaccines.
Common side effects linked to the HPV vaccine mirror those seen with other vaccines and include temporary pain at the injection site, mild fever, dizziness, and headaches. These side effects are typically mild and self-resolve without the need for medical intervention.
There have been concerns that the HPV vaccine might be associated with serious health issues, such as Guillain-Barre Syndrome (GBS), an uncommon condition characterized by the immune system attacking the nerves. Extensive research, however, has not found consistent evidence indicating an increased risk of GBS due to the vaccine.
Long-term safety of the HPV vaccine has been the subject of comprehensive study, with follow-up investigations spanning over a decade. These studies have consistently shown no significant long-term safety concerns. Continuous monitoring remains in place to promptly identify and address any rare side effects.
The vaccine has also undergone scrutiny for a potential link to autoimmune disorders. Large-scale studies involving millions of vaccinated individuals have failed to establish a causal connection between the HPV vaccine and autoimmune diseases.
Regarding fertility concerns, research has demonstrated that the HPV vaccine does not negatively impact fertility. In fact, it may indirectly safeguard fertility by preventing HPV-related diseases.
On a global scale, the World Health Organization (WHO) has repeatedly endorsed the safety and efficacy of the HPV vaccine. The vaccine is widely used in numerous countries worldwide, with international health organizations maintaining continuous safety data monitoring.
Another crucial aspect of safety pertains to the vaccine's composition. HPV vaccines do not contain live virus, DNA, or materials capable of causing HPV infection or cancer. Instead, they consist of virus-like particles meticulously designed to stimulate an immune response.
Before obtaining approval, the HPV vaccine underwent thorough testing in clinical trials encompassing thousands of participants. Subsequent to approval, it has remained subject to ongoing monitoring and research, reaffirming its robust safety profile. Public health authorities worldwide persist in their vigilance, ensuring that the HPV vaccine continues to serve as a secure and effective tool in preventing HPV-related diseases.
Can Males Also Receive the HPV Vaccine?
The question of whether males can receive the Human Papillomavirus (HPV) vaccine is crucial for cancer prevention. Initially targeted at females due to its association with cervical cancer, evolving recommendations now recognize HPV's impact on males.
HPV is a gender-neutral virus, affecting both sexes and contributing to various health issues in males, including genital warts, penile, anal, and oropharyngeal cancers. As a result, health authorities now recommend the HPV vaccine for males.
The Centers for Disease Control and Prevention (CDC) advises boys to receive the HPV vaccine at around age 11 or 12, as it is most effective when administered before potential exposure to HPV, often occurring through sexual contact.
For males who missed vaccination in early adolescence, catch-up vaccination is recommended up to age 21 to ensure protection against HPV-related diseases they may encounter later in life.
The HPV vaccine offers dual benefits for males. First, it directly safeguards them against HPV-related health issues. Second, by reducing the overall prevalence of HPV, it indirectly protects their sexual partners, contributing to broader public health benefits.
Men who have sex with men (MSM) and transgender individuals are especially encouraged to receive the HPV vaccine. These groups face an elevated risk of HPV-related diseases, making vaccination a critical preventive measure.
Extensive research has documented the safety and efficacy of the HPV vaccine in males. Clinical trials and studies have shown that the vaccine is highly effective in preventing genital warts and precancerous conditions in males, with a safety profile similar to that observed in females.
In the context of herd immunity, vaccinating both males and females is essential. When a significant portion of the population is immunized against HPV, the spread of the virus is significantly curtailed, benefiting even those who are not directly vaccinated.
Despite the clear advantages, there remains a gap in HPV vaccination rates between males and females. Ongoing public health campaigns and educational efforts aim to raise awareness about the importance of vaccinating males against HPV.
How Effective Is the HPV Vaccine?
Since its introduction, the effectiveness of the Human Papillomavirus (HPV) vaccine in preventing HPV-related diseases has been a subject of extensive research and analysis. This vaccine is specifically designed to target various HPV strains, which are primary culprits behind cervical cancer, other cancer types, and genital warts. Assessing the vaccine's efficacy is pivotal for its role in public health.
Multiple studies have consistently demonstrated that the HPV vaccine is remarkably effective in thwarting infections caused by the HPV strains covered by the vaccine. Notably, vaccines like Gardasil 9 provide robust protection against the HPV strains most commonly associated with cervical cancer and genital warts.
A crucial gauge of the vaccine's effectiveness lies in its ability to significantly reduce the occurrence of cervical precancerous lesions among vaccinated populations. This reduction signals a tangible decrease in the risk of developing cervical cancer later in life.
Furthermore, the HPV vaccine has exhibited high efficacy in preventing genital warts. Nations with high HPV vaccination rates have reported substantial declines in genital warts cases, not only among vaccinated individuals but also among those who haven't received the vaccine. This suggests the presence of a herd immunity effect.
For the vaccine to be most effective, it is strongly recommended to administer it before individuals become sexually active. This is because the vaccine's purpose is preventive, not curative, meaning it cannot treat existing HPV infections.
Long-term studies have shown that the protection offered by the HPV vaccine against HPV infections endures for many years after vaccination. Although the exact duration of this protection is still being explored, the vaccine's long-lasting effects are evident.
Moreover, research has confirmed the vaccine's effectiveness in males, as it prevents genital warts and anal precancers. This substantiates the recommendation for both males and females to receive the vaccine.
While the HPV vaccine is highly effective against the specific HPV strains it targets, it is important to note that it does not provide protection against all HPV types. Therefore, continued cervical cancer screening practices, such as Pap smears, remain crucial even for vaccinated individuals.
Furthermore, ongoing research is investigating the vaccine's effectiveness in older populations who receive it later in life. While the vaccine is most advantageous when administered at a younger age, it can still offer protection to older individuals who have not been exposed to the HPV types covered by the vaccine.
At What Age Should the HPV Vaccine Be Given?
Determining the best age for administering the Human Papillomavirus (HPV) vaccine is essential for maximizing its effectiveness in preventing HPV-related diseases like cancers and genital warts.
The CDC advises initiating HPV vaccination at around 11-12 years of age. This timing offers significant advantages, including a more robust immune response and reduced potential HPV exposure before the onset of sexual activity.
Starting the vaccine as early as age 9 is also a viable option, ensuring completion well before sexual activity begins.
For those who missed vaccination at the recommended age, catch-up vaccination is recommended. Females can receive the vaccine up to age 26, while males can do so up to age 21 (or up to age 26 for specific high-risk groups).
It's crucial not to overlook males, as they gain protection against HPV-related diseases and contribute to overall herd immunity.
In certain circumstances, vaccination after age 26 may be advisable, necessitating a discussion with a healthcare provider.
For individuals commencing the series before age 15, two doses generally suffice, while those aged 15 and older require a three-dose series for comprehensive protection.
Pregnant women are typically advised to delay HPV vaccination until after pregnancy, with no evidence of harm to the fetus.
The ultimate goal of the HPV vaccine is to shield individuals before HPV exposure. Adhering to the recommended age guidelines ensures effective, long-lasting protection against a range of HPV-related health concerns.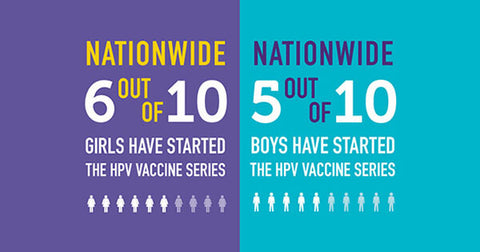
Can the HPV Vaccine Cause HPV?
One common concern regarding the Human Papillomavirus (HPV) vaccine revolves around whether it can lead to an HPV infection. This apprehension arises from a misunderstanding of vaccine composition and function. To alleviate these concerns, it's crucial to clarify the HPV vaccine's components and how it operates.
The HPV vaccine, employed to prevent cervical cancer, other cancers, and genital warts, does not contain any live or inactivated HPV virus. Instead, it utilizes a protein that mimics the virus. This fundamental distinction explains why it cannot trigger an HPV infection.
The vaccine relies on virus-like particles (VLPs), meticulously crafted to resemble the HPV virus. These VLPs prompt the immune system to recognize and develop defenses against the virus. However, VLPs lack the vital DNA necessary for infectiousness.
Since the HPV vaccine lacks any elements that can induce HPV, any subsequent HPV infection following vaccination is unrelated to the vaccine itself. It's more likely due to prior exposure to the virus before vaccination or during the period before the vaccine provides complete protection.
It's essential to grasp that the HPV vaccine is a preventive measure, not a treatment. It thwarts future HPV infections but doesn't address existing infections or HPV-related diseases. Consequently, an individual might still test positive for HPV after vaccination if they were infected before receiving the vaccine.
The misconception that vaccines can cause the diseases they guard against is not unique to the HPV vaccine. However, this fallacy has been debunked by a plethora of scientific studies and the consensus of healthcare experts across various vaccine types.
Before the HPV vaccine received approval, rigorous clinical trials were conducted, which found no evidence of the vaccine causing HPV infection among participants. These trials are vital in ensuring the vaccine's safety and efficacy.
Continuous monitoring and research have been ongoing since the HPV vaccine's introduction. These studies consistently reinforce the conclusion that the vaccine is safe and does not induce HPV or increase the risk of HPV-related diseases.
Educational initiatives are vital for dispelling myths and misconceptions about the HPV vaccine. Healthcare providers play a pivotal role in providing accurate information about the vaccine's safety and effectiveness.
Can the HPV Vaccine Prevent Cervical Cancer?
The HPV vaccine represents a significant breakthrough in the battle against cervical cancer, which is mainly triggered by certain HPV strains. It effectively targets high-risk HPV types, including 16 and 18, known culprits behind most cervical cancer cases, reducing the risk of infection.
The vaccine's wide usage has led to a notable decrease in cervical precancers, the precursors to cancer, underscoring its effectiveness. To maximize its benefits, it's most advantageous when given before sexual activity commences, preventing initial HPV exposure.
Countries with robust vaccination programs have witnessed marked declines in cervical cancer rates, particularly among the age groups they target, demonstrating the vaccine's role in population-level cancer prevention.
However, it's vital to understand that the vaccine doesn't provide immunity against all HPV types that can lead to cervical cancer. Therefore, regular cervical cancer screenings, such as Pap tests and HPV tests, remain essential for vaccinated individuals.
Current evidence suggests that the HPV vaccine offers long-lasting protection against cervical cancer.
To achieve maximum impact in reducing cervical cancer rates, it is crucial to attain widespread vaccine coverage, necessitating comprehensive public health campaigns and educational efforts to boost vaccination rates.
Focusing on vaccinating both girls and boys helps curb HPV transmission, indirectly protecting against cervical cancer and other HPV-related diseases.
The HPV vaccine's safety and efficacy have positioned it as a cornerstone of global public health strategies, offering significant potential to alleviate the global burden of cervical cancer.
Is the HPV Vaccine Necessary If I Am Already Sexually Active?
There's a common question about the HPV vaccine's necessity for sexually active individuals. Some believe it's only effective before sexual activity starts, but this isn't entirely accurate. The vaccine remains valuable for those already sexually active.
The HPV vaccine covers multiple HPV strains, offering protection against types individuals may not have encountered. Even if someone's been exposed to one type, the vaccine can protect against others it covers.
For sexually active individuals, the vaccine still provides benefits in guarding against HPV-related diseases like certain cancers and genital warts. While it's most effective before sexual activity begins, it still offers considerable post-exposure benefits.
Many sexually active people may not have encountered all the HPV types the vaccine addresses. So, vaccination can provide protection against unencountered strains, reducing future health risks.
Moreover, HPV can spread through various sexual activities, not just penetrative sex. The vaccine shields against HPV strains transmitted through genital skin-to-skin contact in various sexual encounters.
People might not always know if they have an HPV infection, as it often lacks symptoms. Vaccination offers peace of mind by preventing future infections with high-risk HPV types.
The CDC recommends the HPV vaccine for all up to age 26, regardless of sexual activity. This highlights its importance, even for sexually active individuals.
For older sexually active people, consulting a healthcare provider can help decide whether to get the vaccine. While typically recommended up to 26, specific circumstances may warrant vaccination for older individuals.
Considering potential future sexual partners is also crucial. The HPV vaccine continues to offer protection as sexual activity evolves, including safeguarding against previously unencountered strains.
Lastly, vaccination contributes to public health by reducing overall HPV prevalence. By getting vaccinated, sexually active individuals protect themselves and help lower HPV transmission rates, benefiting the community's health.
Does the HPV Vaccine Protect Against All Types of HPV?
The HPV vaccine is a crucial advancement in preventive healthcare, targeting specific HPV types. HPV includes over 200 related viruses, with around 40 affecting the genital area. However, it's vital to note that the vaccine doesn't encompass all HPV types.
Vaccines like Gardasil 9, Gardasil, and Cervarix focus on particular virus strains. Gardasil 9, for instance, guards against nine common HPV types linked to cervical cancer and genital warts.
HPV types 16 and 18 cause most cervical cancers worldwide. Available vaccines offer strong protection against these high-risk types, significantly reducing cervical cancer risk.
Gardasil 9 also shields against seven other HPV types (6, 11, 31, 33, 45, 52, and 58) associated with cancers and genital warts.
While highly effective against the covered types, the vaccine doesn't shield against all HPV strains, leaving vaccinated individuals at risk for other HPV infections.
The inclusion of specific HPV types in the vaccine is based on their prevalence and cancer association, focusing on those commonly linked to HPV-related cancers and genital warts.
For protection against non-vaccine HPV types, safe sex and regular screenings (like Pap tests) are crucial for detecting and managing related health issues.
Completing the vaccine series significantly enhances protection against the covered types, reducing HPV-related disease incidence.
Ongoing research aims to develop vaccines covering more HPV types to broaden protection and reduce related diseases.
The vaccine's effectiveness against covered types contributes to herd immunity, reducing their spread and indirectly protecting against non-vaccine types.
Is the HPV Vaccine Free of Cost?
The availability and cost of the Human Papillomavirus (HPV) vaccine can vary depending on location, healthcare systems, and insurance coverage. Many countries have implemented strategies to make the vaccine affordable or free as part of their public health initiatives.
In the United States, the Vaccines for Children (VFC) program provides free HPV vaccines to eligible children and adolescents who are uninsured, underinsured, on Medicaid, or belong to American Indian or Alaska Native communities. Additionally, the Affordable Care Act mandates that most private health insurance plans cover the HPV vaccine at no cost when administered by in-network providers.
Several European nations incorporate the HPV vaccine into their national immunization programs, offering it free of charge to the specified age group.
Countries with universal healthcare systems, such as Canada and the United Kingdom, typically provide the HPV vaccine for free as a routine part of their immunization schedules for children and adolescents.
In regions where vaccine cost is a barrier, initiatives and negotiations with manufacturers aim to reduce the vaccine's price and increase affordability.
Global health organizations like the World Health Organization (WHO) and GAVI, the Vaccine Alliance, strive to enhance accessibility to vaccines like HPV in lower-income countries, often by subsidizing costs or providing them for free.
Despite these efforts, disparities in vaccine access and cost persist worldwide. In certain countries, individuals may have to pay for the HPV vaccine out-of-pocket if it is not covered by their national healthcare system or insurance plan.
Community health centers and public health clinics may offer the HPV vaccine at reduced prices or for free, particularly to underserved populations.
Individuals considering the HPV vaccine should explore their options and inquire about their insurance coverage to access the vaccine at minimal or no cost, as resources are often available to facilitate affordability.
Can I Get the HPV Vaccine If I Already Have HPV?
Many wonder if the HPV vaccine is relevant after contracting HPV. While it doesn't treat existing infections, it can still offer benefits.
The vaccine guards against several harmful HPV strains. So even if you have one type, it can protect against others you haven't encountered.
For those with HPV-related health issues, like genital warts or cervical precancerous lesions, it can prevent future infections causing similar problems.
The CDC recommends the HPV vaccine for those up to age 26, regardless of prior HPV exposure.
Even if you've had HPV, it's unlikely you've encountered all covered by the vaccine, providing additional protection.
Sexually active adults who haven't been vaccinated can discuss its benefits with a healthcare provider.
For those with a history of HPV-related cancers or diseases, the vaccine offers secondary prevention.
Remember, the vaccine is most effective before HPV exposure, but it still benefits those already exposed.
How Long Does the HPV Vaccine Last?
Research indicates that the HPV vaccine offers extended protection against HPV-related diseases. Studies show its effectiveness for at least 10 years, with no significant decline observed. Antibody levels in vaccinated individuals remain consistently high, suggesting enduring immunity.
While the precise duration of protection is still under investigation, ongoing research explores the possibility of future booster shots. This long-lasting immunity is particularly important since the vaccine is typically administered to preteens and teenagers.
When compared to other vaccines, there are indications that the HPV vaccine may provide lifelong protection. Public health organizations like the CDC and WHO continually monitor its effectiveness, updating guidelines as necessary.
It's important to note that for those who received the vaccine more than a decade ago, there is currently no recommendation for a booster HPV vaccine shot. This decision is based on the sustained effectiveness observed in long-term studies.
What Are the Ingredients in the HPV Vaccine?
The HPV vaccine, crucial for preventing certain cancers and genital warts, contains specific ingredients serving distinct roles. Key components include virus-like particles (VLPs), which mimic HPV's outer shell, and adjuvants like aluminum salts to enhance the immune response. Stabilizers maintain the vaccine's efficacy during storage, and some formulations include preservatives for safety. Yeast cells are used to produce VLPs, and saline dilutes the vaccine for administration. While trace yeast proteins may be present, the vaccine undergoes rigorous testing for safety and effectiveness to ensure robust protection against HPV with minimal side effects.
Can the HPV Vaccine Help If I Already Have Genital Warts?
The HPV vaccine's effectiveness for individuals with genital warts is an important consideration. Genital warts result from certain HPV strains, but the vaccine's primary role is prevention, not treatment.
While the vaccine won't cure or directly affect existing warts, it remains beneficial. It provides protection against other HPV strains, reducing the risk of additional complications. This is significant because individuals can be infected with multiple HPV types.
Additionally, the vaccine can prevent future wart outbreaks by safeguarding against the responsible strains. It's particularly valuable in protecting against HPV strains associated with various cancers.
Public health guidelines suggest the vaccine for individuals up to age 26, encompassing those exposed to HPV or with genital warts. Deciding to vaccinate should involve discussing health status and risks with a healthcare provider.
Is the HPV Vaccine Only for Females?
The HPV vaccine, once primarily considered for females, is equally important for males. HPV affects both genders, causing genital warts and various cancers. Including males in vaccination efforts is essential for comprehensive HPV prevention.
Initially, the focus was on females due to the link between HPV and cervical cancer. As more information emerged, it became evident that males also face HPV-related health risks.
Health organizations like the CDC recommend HPV vaccination for both boys and girls, usually around age 11 or 12 but starting as early as 9.
Vaccinating males not only protects them but also contributes to herd immunity, reducing overall virus prevalence and protecting the unvaccinated.
For men who have sex with men (MSM), the vaccine is crucial as they face higher HPV-related disease risks, especially anal cancer.
By vaccinating all genders, HPV spread decreases, lowering related disease rates for everyone.
Studies confirm the vaccine's safety and efficacy for males, preventing genital warts and anal cancers, with ongoing research examining its impact on other HPV-related conditions.
Despite these benefits, vaccination rates for males lag behind females. Efforts to raise awareness and acceptance among males are crucial.
In conclusion, the HPV vaccine is vital for both females and males, protecting against various HPV-related health issues and aiding broader HPV control efforts.
Can Pregnant Women Receive the HPV Vaccine?
Health guidelines, such as those from the CDC, advise against administering the HPV vaccine during pregnancy. This precautionary measure is due to limited research on the vaccine's impact on pregnant women and developing fetuses, not because of known risks. If a woman becomes pregnant during the HPV vaccine series, the remaining doses are typically postponed. Importantly, receiving a vaccine dose unknowingly during pregnancy is not considered concerning, though consultation with a healthcare provider is advisable. Pregnant women interested in HPV vaccination are encouraged to wait until after childbirth. Decisions regarding vaccination timing should involve a discussion with a healthcare professional, taking into account individual health, risk factors, and medical history. For those planning a pregnancy, completing the HPV vaccine series before conceiving is a prudent choice. Ongoing research may provide clearer guidance on HPV vaccination's safety and efficacy during pregnancy.