Human Papillomavirus (HPV) is one of the most common sexually transmitted infections (STIs) globally, affecting millions of people each year. While HPV is widely recognized for its link to cervical cancer and other health issues, it is also surrounded by misconceptions and stigma. One of the most controversial questions that arises is: Is HPV a sign of cheating? This article delves into the complexities of HPV, its transmission, and the relationship dynamics it may impact. By addressing this sensitive topic, we aim to provide clarity, dispel myths, and offer guidance for those navigating this challenging situation.
What is HPV?
HPV is a group of more than 200 related viruses, some of which are sexually transmitted. It is so common that nearly all sexually active individuals will contract at least one type of HPV at some point in their lives. The virus is categorized into two main types:
-
Low-risk HPV: These strains may cause genital warts but are not associated with cancer.
-
High-risk HPV: These strains can lead to cancers of the cervix, anus, throat, and other areas.
HPV is transmitted through intimate skin-to-skin contact, primarily during vaginal, anal, or oral sex. It can also be spread through non-penetrative sexual activities. Importantly, HPV can remain dormant in the body for years, making it difficult to determine when or from whom the infection was contracted.
Can HPV Indicate Cheating?
The question of whether HPV is a sign of cheating is complex and emotionally charged. To answer this, we need to consider several factors:
1. HPV Can Remain Dormant for Years
One of the most critical aspects of HPV is its ability to lie dormant in the body for extended periods—sometimes even decades. This means that a person diagnosed with HPV may have contracted the virus long before their current relationship began. Therefore, a diagnosis does not necessarily indicate recent infidelity.
2. HPV is Extremely Common
Given its prevalence, HPV is not a reliable indicator of cheating. Most sexually active individuals will contract HPV at some point, often without knowing it. The virus can be transmitted even when no symptoms are present, making it challenging to trace its origin.
3. Previous Relationships and Sexual History
A person’s sexual history, including past relationships, can play a significant role in HPV transmission. If either partner has had previous sexual encounters, they may have contracted HPV long before their current relationship. This further complicates the assumption that HPV is a sign of cheating.
4. False Assumptions and Stigma
The stigma surrounding STIs often leads to false assumptions about fidelity. Accusing a partner of cheating based on an HPV diagnosis can damage trust and create unnecessary conflict. It is essential to approach the situation with empathy and understanding rather than jumping to conclusions.
How to Approach the Conversation About HPV
If you or your partner has been diagnosed with HPV, it’s crucial to handle the situation with care. Here are some tips for navigating this sensitive topic:
1. Educate Yourself
Before discussing HPV with your partner, take the time to educate yourself about the virus. Understanding how HPV is transmitted, its prevalence, and its potential health implications can help you approach the conversation with confidence and clarity.
2. Choose the Right Time and Place
Timing and setting are critical when discussing sensitive topics. Choose a private, comfortable environment where both of you can speak openly without distractions or interruptions.
3. Be Honest and Transparent
Honesty is key when discussing HPV. Share your diagnosis with your partner and encourage them to do the same. Transparency can help build trust and foster a sense of teamwork in addressing the issue.
4. Avoid Blame and Accusations
It’s natural to feel upset or confused after an HPV diagnosis, but blaming or accusing your partner will only create tension. Instead, focus on finding solutions and supporting each other through the process.
5. Seek Professional Guidance
If you’re struggling to navigate the conversation, consider seeking guidance from a healthcare professional or counselor. They can provide valuable insights and help mediate the discussion if needed.
Preventing HPV Transmission
While HPV is highly contagious, there are steps you can take to reduce the risk of transmission:
1. Get Vaccinated
The HPV vaccine is highly effective in preventing infection with the most common high-risk and low-risk strains of the virus. The vaccine is recommended for both males and females, ideally before becoming sexually active.
2. Practice Safe Sex
Using condoms or dental dams during sexual activity can reduce the risk of HPV transmission. However, it’s important to note that HPV can infect areas not covered by protection, so safe sex practices are not foolproof.
3. Regular Screenings
Regular cervical cancer screenings, such as Pap smears and HPV tests, can help detect high-risk HPV strains early and prevent complications. Men should also be aware of their HPV status, although there is no routine screening for males.
4. Open Communication
Discussing sexual health with your partner is essential for preventing STIs. Regular check-ups and honest conversations about sexual history can help you both stay informed and protected.
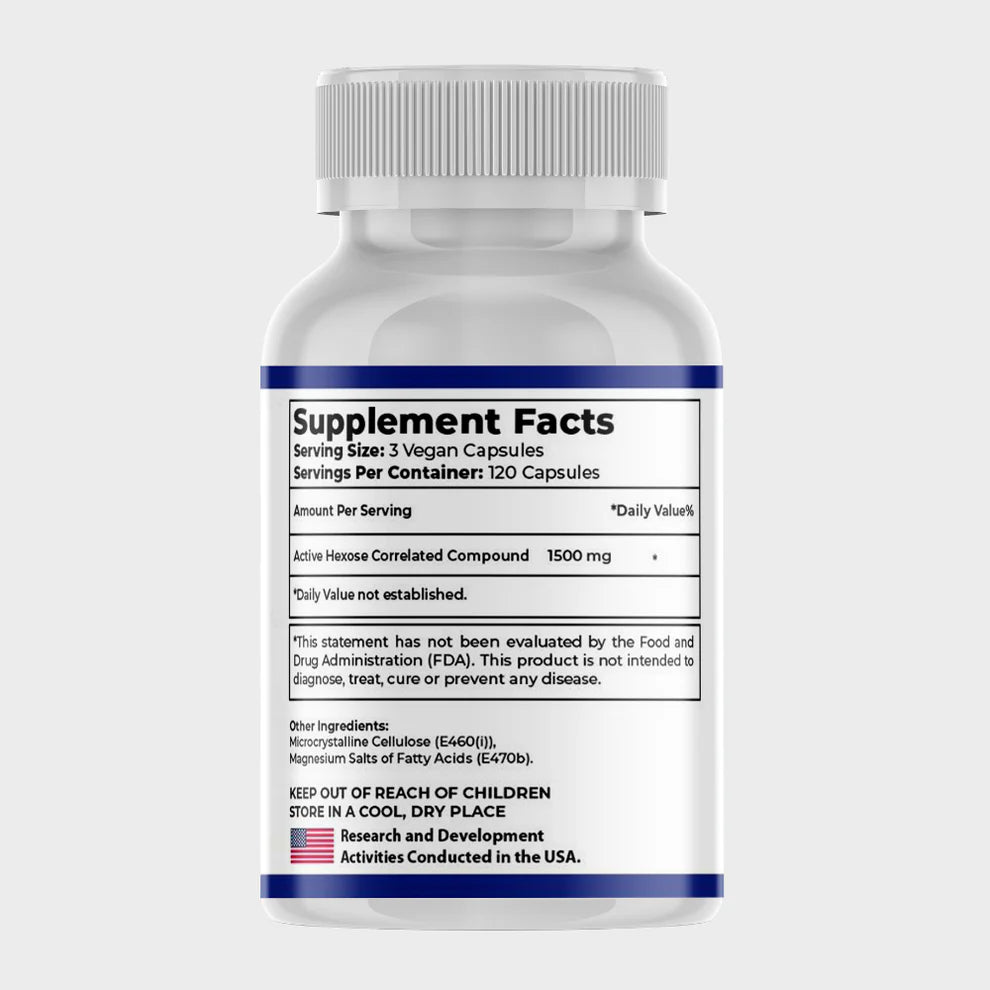
5. Consider AHCC Supplement
Active Hexose Correlated Compound (AHCC) is a natural supplement derived from medicinal mushrooms, known for its immune-boosting properties. Research has shown that AHCC can be effective in supporting the body's ability to clear HPV infections. In fact, studies have demonstrated that consistent use of AHCC supplements for six months has proven to help eliminate HPV in many cases, making it a promising option for those managing the virus
The Emotional Impact of an HPV Diagnosis
An HPV diagnosis can be emotionally challenging for both partners. Feelings of guilt, shame, anger, and confusion are common. Here’s how to cope:
1. Acknowledge Your Emotions
It’s normal to experience a range of emotions after an HPV diagnosis. Allow yourself to process these feelings without judgment.
2. Lean on Your Support System
Reach out to trusted friends, family members, or support groups for emotional support. Sharing your experience with others who understand can be incredibly comforting.
3. Focus on the Facts
Remind yourself that HPV is a common virus and not a reflection of your character or relationship. Focusing on the facts can help alleviate unnecessary guilt or anxiety.
4. Seek Professional Help
If you’re struggling to cope with the emotional impact of an HPV diagnosis, consider speaking with a therapist or counselor. They can help you work through your feelings and develop healthy coping mechanisms.
Debunking Common Myths About HPV
Misinformation about HPV can contribute to stigma and misunderstandings. Let’s debunk some common myths:
1. Myth: Only Promiscuous People Get HPV
Fact: HPV is so common that almost everyone who is sexually active will contract it at some point, regardless of the number of partners they’ve had.
2. Myth: HPV Always Causes Symptoms
Fact: Many people with HPV never develop symptoms and may not even know they’re infected.
3. Myth: HPV is a Life Sentence
Fact: Most HPV infections clear on their own within two years without causing any health problems.
4. Myth: HPV Only Affects Women
Fact: HPV can affect both men and women and is linked to various cancers in both sexes.
Conclusion: HPV is Not a Sign of Cheating
In conclusion, an HPV diagnosis is not a definitive sign of cheating. The virus’s ability to remain dormant for years, its high prevalence, and the complexities of sexual history make it impossible to pinpoint its origin with certainty. Instead of focusing on blame, couples should prioritize open communication, education, and preventive measures to protect their health and strengthen their relationship.
If you or your partner has been diagnosed with HPV, remember that you are not alone. With the right support and information, you can navigate this challenge together and emerge stronger than ever. By dispelling myths and fostering understanding, we can reduce the stigma surrounding HPV and promote healthier, more informed conversations about sexual health.